×
- Services
- Resources
- Careers
- About Us
- Appointments
We Care. We Save Lives.
We are Western Colorado’s behavioral health care leader serving our communities since 1972.
A Message from our President & CEO and Board Chairman,
As we reflect on not only the ending of a fiscal year but an entire decade, it is with appreciation and gratitude that we embrace the past and look towards the challenges and goals ahead.
We Save Lives. In the changeable world this is a constant for us – past, present and future. In the midst of last fiscal year’s unpredictability, great bridges were built over uncertain waters and connected Coloradans to new and innovative treatments and services. Together we have made noteworthy progress in transforming behavioral health care on the Western Slope.
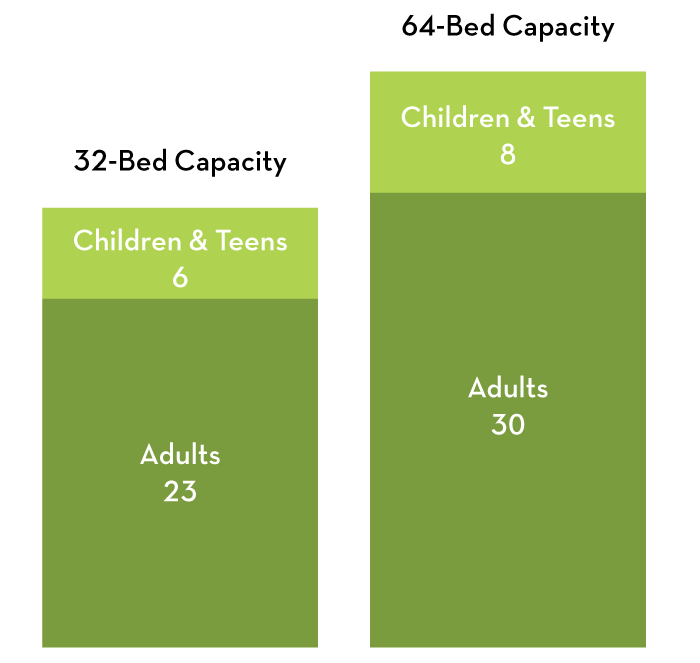
With your support this past year, the new West Springs Hospital opened its beautiful and trauma-informed new doors to twice as many patients as before, making a real impact in alleviating local suffering. With the new 63,000 sq.ft. hospital open, our crisis stabilization unit, Transitions at West Springs, itself transitioned to become incorporated within the hospital, as did walk-in crisis services.
Mind Springs Health innovated an impactful, new treatment program for clients and rolled it out to all outpatient offices in our 10-county service area. ‘Phase-based care’ received national commendation, with awards and presentations at multiple industry conferences. Medication-assisted therapy programs expanded, and Mind Springs Health introduced Summit County to horticultural therapy for the first time.
Here is the story of our Fiscal Year 2018-2019. It’s a story of better care, better world.
With appreciation and gratitude,
Sharon Raggio, LPC LMFT MBA
President & CEO
Bill Anuszewski, MBA
Boards of Directors Chairman
It has changed the face of psychiatric treatment on the Western Slope, and now, with up to 64 beds, has capacity to provide immediate help to all those in need of its services with a world-class, state-of-the-art custom-designed healing environment. No longer do people unnecessarily suffer in unsafe places waiting for a bed to open up at the only psychiatric hospital on the Western Slope.
Brought to Tears: On Patient Moving Day, a male patient moving from the old hospital into the new one stopped, began looking at the new space, and started to cry. The nurse accompanying him asked why, and he told her it was because he was so shocked at what a beautiful place we had built for him and others like him who need hospitalization and psychiatric help; that he didn’t think anyone really cared about people who need help and he was grateful for what we had done. Recovering his composure, he expressed the desire to get well so he could work for us one day.
A Standing O: Two days after Moving Day during the first Saturday evening dinner in the new hospital, all of the patients and staff dining suddenly rose and gave a spontaneous standing ovation to the kitchen team for the quality of the food and friendliness of the staff.
A Breath of Fresh Air: Regardless of weather, year-round the outdoor courtyard areas are being used by the adult patients to walk, think or just sit and rest!
A Heartfelt Thank You: One day our Vice President of Philanthropy Roger Sheffield was in the dining room when a female patient came over to him and asked him who he was. He told her about his role in making the new hospital a reality. She then shook his hand, hugged him, thanked him for the new building and for the dining room area, and told him the food was wonderful!
Designed for Safety: An adult male attempted to harm himself using his clothing and his bedroom door. The thoughtfully-planned safety system activated as designed, with the overhead door sensor immediately sounding, the light above the door indicating where the problem was, and the alarm at the care team station alerting staff, who immediately responded and interrupted the attempt. Staff describe the units as welcoming and an enjoyable place to work, and, more importantly, a much safer place for patients.
In the Gym: Site of yoga, Zumba, karaoke, basketball and many other physical activities! Staff are enjoying participating with the patients. It also was used recently for a several-hour lockdown, providing safe space & shelter for nearly 100 staff and outpatient clients for shelter and safety. The Kitchen provided snacks and refreshments during this stressful time– before the new hospital, this wouldn’t have been possible
“…is a wonderful Lady. She treated me with utmost respect and I can’t say enough about her. She is very professional and helpful!! She is a rare find for sure and West Springs Hospital is fortunate to have her!!!”
“…is a breath of joy and happy all the time and I appreciate that very much!! I feel blessed to be cared for by all these people!!”
“…is one of the best and most valuable Mental Health Workers this hospital has to offer. He has been there for me over the years when I was at my absolute worst and he has given me the best and most uplifting advice.”
“…such an upbeat person, she is always smiling and full of joy and happiness, which is very contagious and that is awesome!!”
“What a wonderful human being. Very kind. Very self-disciplined! He helped me with my medication sheet so I could stay up on them and that meant the world to me! Thank you!”
“…has always treated me with respect every single time I have asked a question or asked him to help me with something. He is very professional about it all the time and I appreciate that very much.”
Designed By
Davis Partnership Architects
Hospital Patients & Staff
Built By
FCI Constructors
Financed in Part By
Bank of the San Juans
Owners Represented By
Robert D. Jenkins, AIA

Limited access and long wait times for psychiatric treatment in the U.S. are vexing problems. Nationally Medicaid patients often wait 7 weeks or more for an initial appointment. Treatment delays contribute to increased morbidity, disability, and potentially, suicide. We have seen a 50% surge in hospital emergency department visits over the last 10 years, with more than 6 million visits annually identifying a psychiatric crisis as the primary complaint.
Typically in Community Mental Health Centers like Mind Springs Health, pharmacotherapy and psychotherapy work independently, and inclusion of peers and case managers in treatment are “as needed”. Patient choice of treatment modalities cannot always be accommodated with clinic workflows and protocols, and appointments are most often determined by staff schedules (which are typically saturated), rather than clinical acuity or need. Treatment delays and inadequate intensity contribute to poor compliance and inadequate responses. Financial limitations and staff shortages required that novel approaches to care were explored.
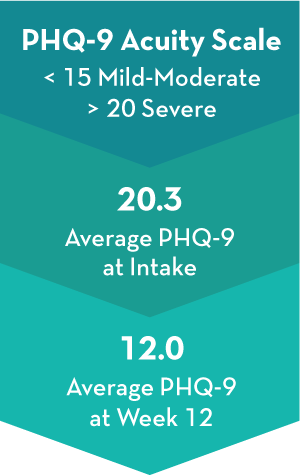
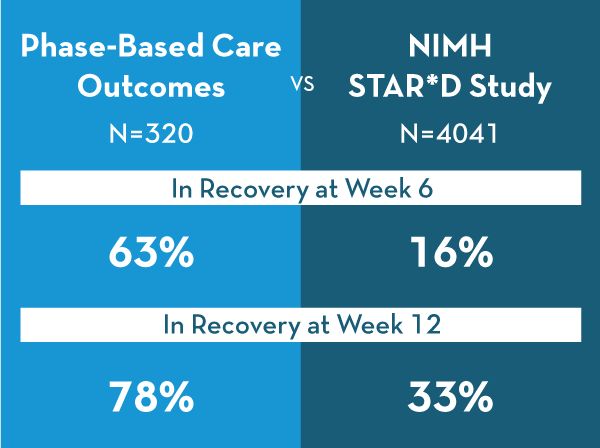
To address these challenges of access, resource limitations, and patient engagement, we unencumbered ourselves of restrictive processes and thinking, and focused on innovating along core organizational values – person-centered care, evidence-based care, fiscal effectiveness, positive work environment. In doing so, we acknowledged there are “phases” to most patients’ illnesses as they move between different acuity states. Thus, Mind Springs Health’s Phase-based Care program began, with a goal to improve both clinical outcomes and patient engagement.
Developed by Chief Medical Officer Jules Rosen MD, Quality & Assurance Vice President David Hayden LPC, CAC III & Mind Springs Health Executive Vice President Michelle Hoy LPC, CAC III during a year-long Lean Six Sigma process, the program uses mathematical algorithms to help create multi-disciplinary treatment teams of therapists, medical providers, case managers and peers, and proportionately allocate resources towards acute-phase patients who need them the most. Every therapeutic interaction is measured with validated rating instruments specific to the consumer’s symptom profile.
Client outcomes have been nothing short of astounding and by the end of our fiscal year the program was widely available across Mind Springs Health’s 10-county service area.
Bestowed by the Colorado Behavioral Healthcare Council to methodologies, systems or procedures that demonstrate best practices in a clinical arena.
Awarded by a partnership between the Institute for Healthcare Improvement Lucien Leape Institute and Taylor Communications to honor and elevate the innovative work people and organizations from across the continuum of care are doing to advance patient and family engagement.

Dr. Jules Rosen and Phase-Based Care team members
Mental health peers are some of the most important people in our organization. By using their lived experiences with mental illness and recovery, peers provide support and insight that’s based in strength, and are able to reach those struggling in a truly authentic way.
This past year, 2 exceptional peers have opened our eyes and given us a look into living and coping with mental illness. Their unique perspectives have much we can learn from.
 Blogger and author Jill Davis, Colorado Peer and Family Specialist (CPFS) and Coordinator of Mind Springs Health’s Peer Services, has started to gain national and international acclaim for her ‘A Peer’s Perspective’ column about different ways to look at everyday aspects and emotions. It’s not just the content but also the consistency of her biweekly blogs that reach her growing readership base.
Blogger and author Jill Davis, Colorado Peer and Family Specialist (CPFS) and Coordinator of Mind Springs Health’s Peer Services, has started to gain national and international acclaim for her ‘A Peer’s Perspective’ column about different ways to look at everyday aspects and emotions. It’s not just the content but also the consistency of her biweekly blogs that reach her growing readership base.
Mother and volunteer Julie Hart was diagnosed with bipolar disorder just a few years ago although she believes she has been living with it most of her life. Julie has an engaging way of articulating both the intellectual and emotional aspects of living with her diagnosis that gives both great insight into mental illness and powerful tools to fight against the stigma. She calls it ‘Mind Positive’.
Named as one of the Best Doctors in America (only 4% of U.S. physicians receive this honor) for the last 19 years, Chief Medical Officer Jules Rosen MD retired at the end of the fiscal year and leaves an impressive legacy.
He was highly-skilled, compassionate, convivial, and known as an ‘amazing healer’ during the 5 years of his tenure at Mind Springs Health and West Springs Hospital . Regularly going out of his way to consult with the entire health care community, and treating people with complex psychiatric and medical conditions, Dr. Rosen oversaw the expansion of psychiatric services and staff and increased partnerships and programs in primary care practices, hospitals and nursing homes throughout the Western Slope.
Along with Mind Springs Health Executive VP Michelle Hoy and Quality & Compliance VP David Hayden, Dr. Rosen was also a key architect of the award-winning Phase-based care program.
Thank you Dr. Rosen for all you have done for our organization and we look forward to keeping in touch on projects in the future.

Doug Pattison, CPA
A dedicated social services volunteer and philanthropist throughout his life to date, Douglas J. Pattison CPA joined the Mind Springs Health Board in 2017 after relocating to the Western Slope following a long career at Harpo, Inc., the multi-media conglomerate founded by Oprah Winfrey. Energized by what he saw from the Boardroom perspective, Doug assumed the Chief Financial Officer role shortly before fiscal year-end. A graduate of the University of Maryland – University of College, he began his professional career in 1979 at the Federal Bureau of Investigation, and earned his Certified Public Accountant degree in 1986.

Holly Covington, RN PhD PMHNP FNP CNS (Right)
Amongst the many dedicated and talented Colorado hospital professionals, a few stand above the rest in their ability to make a true impact in their hospital and community.
West Springs Hospital’s Holly Covington, RN PhD PMHNP FNP CNS has been honored as one of this year’s elite Colorado Health Care Stars by the Colorado Hospital Association (CHA).
Covington, a hospital Advanced Psychiatric Nurse Provider, was recognized as an exceptional health care professional for superlative patient care, risk-minimization programs, quality assurance, streamlining processes, promoting a positive work place culture and leading by example.
“Holly has provided exceptional care to severely mentally ill individuals for over 20 years” says Kim Boe, Executive Vice President at West Springs who nominated Covington for the award. “She is a leader and applies endless energy toward the health, safety and recovery of psychiatrically-ill individuals.”
Thank you and Congratulations to Holly!
Rural counties across the country like Colorado’s Grand County often experience significant gaps in mental health care which severely impact the overall health of individuals and the community. The Mental Health Navigator program was established in 2016 to remove barriers and assist residents with accessing the mental and behavioral health care services needed.
Mental health care navigators provide direct therapy and counseling as well as connecting individuals and families to other health care services and assisting with transportation needs to keep those service appointments.
This year, Mind Springs Health’s Sue Johnson MSW LSW received the Grand County Rural Health Network’s Excellence in Healthcare Service Award for her exemplary work as a navigator for the community.
Thank you and Congratulations to Sue!

Sue Johnson, MSW, LSW
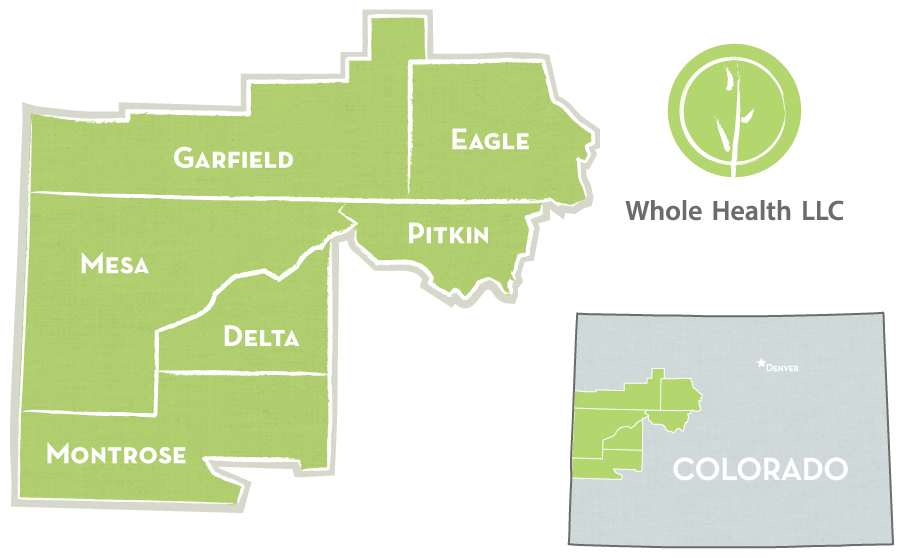
A partnership with Rocky Mountain Health Plans to address behaviors of high Emergency Room utilizers, Whole Health and its team of Community Health Workers have been improving the health of Western Slope residents since 2014. This year, it expanded to 6 counties and was available in Mesa, Garfield, Eagle, Pitkin, Delta & Montrose.
Designed and directed since its inception by Dr. Amy Gallagher, Whole Health’s Community Worker Program is driven by health care’s triple aim:
Participants are selected based upon claims data and/or referrals from medical providers & practices and Rocky Mountain Health Plans, and Community Health Workers, while not providing therapy, use behavioral health techniques to improve the physical health of their clients.
Community health workers partner with individuals to develop health management plans and goals, establish positive relationships, facilitate communication, feedback and access to the social determinants of health and assist in understanding plans, instructions and getting to appointments (very often by providing transportation). The services they provide and the support they offer are a powerful combination in changing behaviors and health for the better. This past year,
*Rocky Mountain Health Plans 2018-19 Data, **Generalized Self-Efficacy Screening Tool, ***Western Colorado Needs Review 2018-19
Changing electronic health record (EHR) systems is never easy. Given the speed of life and technology today, it was a transition we were intent on making so that our organization and, more importantly, those we serve continue to benefit from advanced behavioral health technology and value-based care.

On Day One of the fiscal year, July 1, 2018, Mind Springs Health & West Springs Hospital went ‘live’ with Netsmart’s myAvatar: The EHR for Behavioral Health, culminating over 3 years of work to identify the right EHR for our clients’ & patients’ needs, and then customizing it for our unique, full-continuum of mobile, outpatient and inpatient care. Adopting the new EHR at the beginning of our fiscal year gave our staff some time to adopt and adapt prior to the new hospital opening in December.
myAvatar is specifically designed to provide behavioral health and addictions treatment services in community-based, residential and inpatient programs. It offers a recovery-focused system that leverages real-time analytics and clinical decision support to drive decision-making.
 Its whole-person integrated care model supports roles throughout the organization, from front desk staff and clinicians to administrators and management, resulting in improved operation, clinical and financial workflows for all aspects of our organization.
Its whole-person integrated care model supports roles throughout the organization, from front desk staff and clinicians to administrators and management, resulting in improved operation, clinical and financial workflows for all aspects of our organization.
Mental Health First Aid and Youth Mental Health First Aid are the gold standard in mental illness education and support systems for everyday people. To be certified in one or both of these 8-hour courses that teach how to identify, understand, and respond to signs of mental illnesses and substance use disorders saves lives.
Prior to last year, the Western Slope had just a handful of certified trainers available to provide these courses to the public.

Newly Certified Mental Health First Aid Trainers in Breckenridge
Thanks to grants and support from The Katz-Amsterdam Charitable Trust & Foundation, Pitkin County, Aspen Ski Company’s Caring for the Community Fund and Eagle County/Eagle Valley Behavioral Health, over 80 locally-based individuals have recently been trained as trainers for Mental Health First Aid and Youth Mental Health First Aid in both English and Spanish. With each trainer required to hold 3 trainings a year and up to 30 people in each session, this means that over 7200 local community members have or will learn to assist others.
Find a Course Near You at MindSpringsHealth.org/Mental-Health-First-Aid
The therapeutic benefits of garden environments have long been known, and being close to the earth and participating in the cycle of growth offers many advantages. This is especially true in Mind Springs Health’s Summit County office where Clinician Kristen Greenwald LCSW began 3 horticultural therapy programs this fiscal year – for kids & teens, adults with depression, and adults with post-traumatic stress disorder.
By growing and tending flowers, vegetables and herbs in a sensory garden behind the Mind Springs Health’s office, participants in the program learn emotional regulation and problem-solving skills. Horticultural therapy also can help improve memory, cognitive abilities, task initiation, language skills and socialization.
We are proud to bring this healing program to the Summit County community. Please, step into the garden!
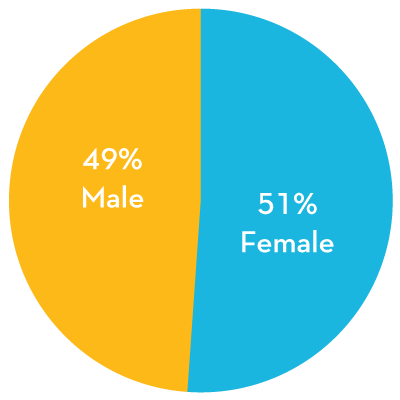
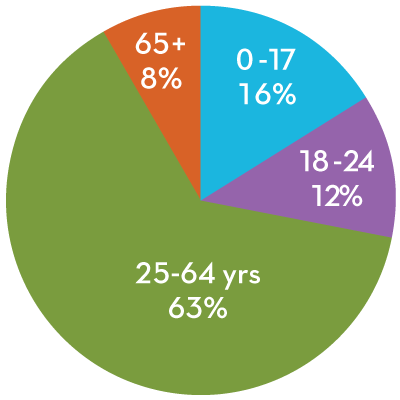
Over 500 strong, our people are our organization and without them there is nothing. In this time of global behavioral health care staff shortages, our employees are among the most skilled and compassionate and it is of the utmost importance to our organizational mission (and a promise to our communities) that we attract and nurture the finest.
Lead by Mind Springs Health EVP Michelle Hoy and Human Resources VP Norma Roberts, recruiting and retaining our staff became an inter-departmental initiative in FY2018-2019 and a multi-tiered program was put into place.
When it comes to recruiting talent, the old strategy of running local newspaper ads no longer works, even here on the Western Slope where local newspapers retain their popularity. With more positions available than people to fill them, competition is national, digital and fierce. We needed to stand out and the strategy was to differentiate ourselves from other mental health organizations through the power of social media & video, personalization of jobs, and desirability of our Western Slope locations.
In addition to being our most valuable asset, there is no one better than our staff to explain why we strive to be the organization of choice for dedicated and motivated health care professionals. Many employees took an active role in recruiting their colleagues by participating in a video campaign where they spoke about job roles, responsibilities and benefits, and our compassionate corporate culture. In the past, we manually promoted open positions on our Facebook and LinkedIn pages and Twitter feed.
We now utilize a digital program to distribute job descriptions and the employee videos across all relevant social media channels, both ones we own (website, Facebook page, Twitter feed) and professional network/recruitment sites like Indeed, Glassdoor and LinkedIn.
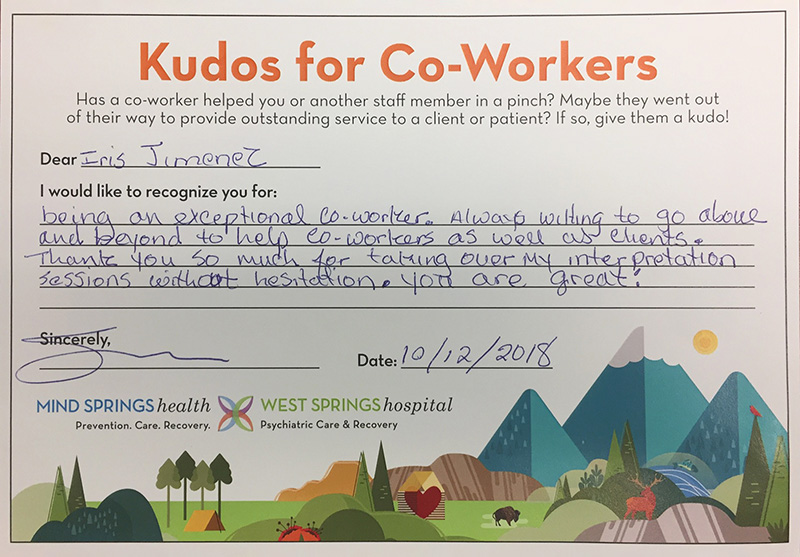
Our organization doesn’t just hire for jobs, we seek mutually-beneficial long-term relationships with our staff. Appreciation, recognition and consistent tokens of thanks are the cornerstones of our efforts to nurture satisfying and productive healthcare careers here.
APPRECIATION – Fostering a culture of literally saying ‘Thank You’ as often as appropriate.
RECOGNITION – Publicizing notable accomplishments both internally and externally, and rewarding outstanding work through the ‘Eagle of Excellence’, ‘Above and Beyond the Call of Duty’ and ‘Customer Service Superstar’ personnel awards.
TOKENS OF THANKS – Small, but meaningful and consistent, gifts to our employees. In the past it has been personalized calendars, this year everyone received a premium aluminum water bottle. A new gifting program for onboarding staff was introduced this year that starts with a welcome basket at New Employee Orientation and delivers different gifts to the employee at their 3-month, 6-month, 1-year and 2-year anniversary. This program complements the one in place that gifts longer-term employees at significant anniversaries.
Eagle, Garfield, Grand, Jackson, Mesa,
Moffat, Pitkin, Rio Blanco, Routt, Summit
Aspen, Craig, Eagle, Glenwood Springs,
Granby, Grand Junction, Meeker,
Rangely, Steamboat Springs




We rebuild lives and inspire hope by providing exceptional mental health and addiction recovery care, strengthening the health and vitality of our communities.
We envision health and wellness in our communities.
Strength Created through Local Partnerships,
with Collaboration and Education
Integrity and Accountability in all we Do
Outcomes-Driven
Responsible Financial Stewardship
Leadership in Physical and Behavioral Health Care
A Culture of Trauma-Informed Care
A Focus on Exceptional Customer Service
The Mind Springs Health Board of Directors and the West Springs Hospital Board of Directors are comprised of a core group of seven directors who serve on both Boards, with four additional directors per board. This past fiscal year Doug Pattison moved off of the Boards when he assumed our CFO role, and we welcomed Grand Junction Police Chief Doug Shoemaker and health care administrators Larry Dupper and Stefan Bate as new members.

Left to Right: Dr. Al Saliman, Larry Dupper, Joan Napolilli, Stefan Bate, Sharon Raggio, Bill Noel, Pat Tucker, Mark Scheel, Stacey Gavrell, Carol Skubic, Bill Anuszewski, Carl Walker. Not Pictured: Doug Shoemaker
Reverend CARL WALKER
Retired
Vail Valley
MARK SCHEEL
Technology
Vail Valley
STEFAN BATE, LAC CCTP
Health care
Roaring Fork Valley
DOUG SHOEMAKER
Law Enforcement
Mesa County
JOAN NAPOLILLI, RN MSN
Health care
Montrose County
STACEY GAVRELL
Health care
Garfield County
LARRY DUPPER
Health care
Garfield County
Similar to our Board structure, a core team provides services and supports across Mind Springs Health, West Springs Hospital and our community health care worker-focused subsidiary Whole Health LLC. Individually there are also organization-specific leaders. Together we inspired, challenged and motivated each other to the fiscal year outcomes seen within this report.

Left to Right: Doug Pattison, Allen Holloway, Norma Roberts, David Hayden, Charles Andrews, Jackie Skramstad, Kim Boe, Brandi Kroese, Dr. Francis Lotrich, Krista McClinton, Michelle Hoy, Dr. Amy Gallagher, Kathy Capps, Sharon Raggio, Felicia Romero, Roger Sheffield, Chriss Flynn, Tom Gangel. Not Pictured: Dr. Jules Rosen
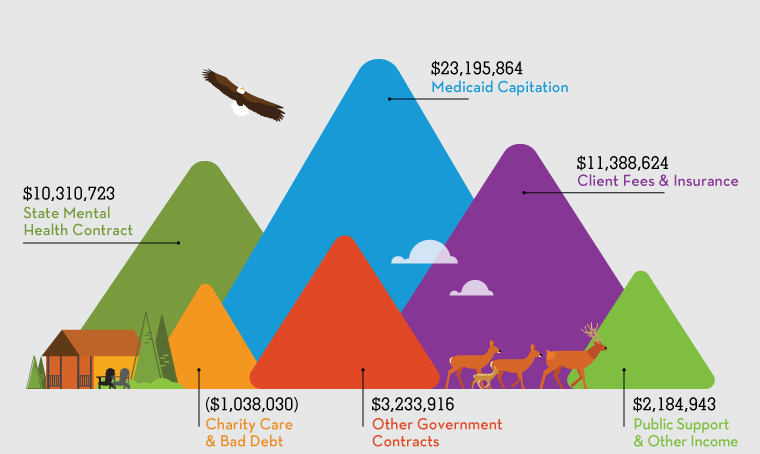
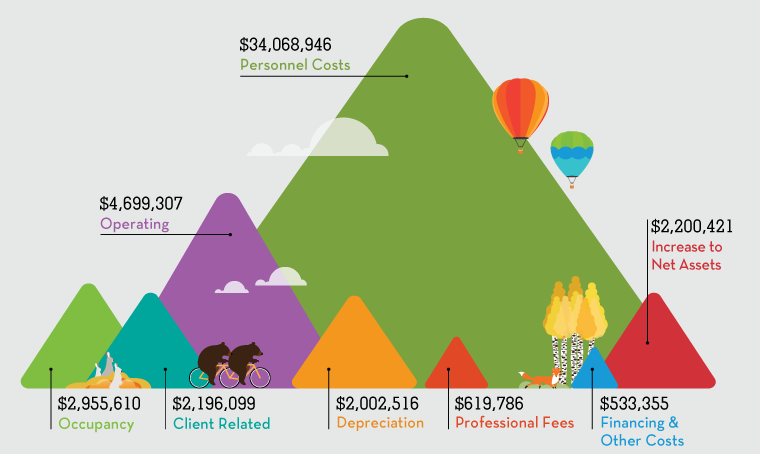
Mind Springs Health and West Springs Hospital are proud to provide our services to all people who need them regardless of their ability to pay, and our organization provides millions of dollars in charity care to the communities we serve every fiscal year. As privately-owned, not for profit entity, we rely upon government and private insurance, and the generosity of donors to cover costs for services provided to the community. And our donors, who are committed not only to our work but also to the cause of behavioral health, are very generous with their time, talents and treasure.
Successful fundraising is essential to our ability to live out our mission of providing quality mental health and addiction care. Building Sanctuary | Rebuilding Lives, the campaign for Mind Springs Health and West Springs Hospital, debuted in 2016 with the initial goal of fundraising $17,750,000 for the new West Springs Hospital’s Phase I construction. With that initial goal successfully reached last December as the new Hospital opened, organizational fundraising objectives have broadened to support a number of outpatient initiatives as well, including the noted expansion of phase-based care and mental health first aid trainer programs.
Honored and humbled by their support, we gratefully recognize all who made a financial gift to Building Sanctuary | Rebuilding lives this past fiscal year.