×
- Services
- Resources
- Careers
- About Us
- Appointments


IMPACT REPORT FOR FISCAL YEAR 2019 – 2020
July 1, 2019 – June 30, 2020
Though the following report covers months prior to the pandemic, it’s hard to remember life back then. Without a doubt, recent times are unprecedented and have challenged all of us as we navigate the worst public health crisis in modern history. As often said, we are all in this together. Thank you for sharing this time of challenge and change.
Our ability to continue to provide life-saving behavioral healthcare was challenged as the virus made its way through Colorado and the nation, and within a matter of days we launched virtual therapy across our service area, allowing us to continue to meet the needs of existing and new clients.
Patience has been challenged as we work in an environment of social distancing, donned with personal protection equipment. Staff resolve is challenged daily, as our dedicated employees interpret and gauge emotional states behind the masks of those requiring in-person treatment. Our resiliency has been challenged as we work through trying times while balancing the obstacles in our personal lives that dealing with the pandemic has brought to all of us. Despite it all, our people have shown an amazing ability to remain focused on doing what they do best – improving and saving lives. Not only have they proven to care for clients with compassion, they care for each other with empathy, kindness and respect.
What has not been challenged, nor ever will be, is our gratitude and appreciation for them, as well as our valued partners and donors. We, like you, persevere. Our mission of rebuilding lives and inspiring hope is too important to do otherwise, and without the perseverance and resiliency of so many we could not be nearly as effective as we are together.
We are grateful for opportunity to share resiliency skills with all of our communities, and feel a deeper connection with so many of you. Thanks for being in this with us!
With Gratitude,
Sharon Raggio, LPC LMFT
President & CEO

Al Saliman, MD
Board Chairman
Life changed dramatically in March 2020 when the coronavirus started to ravage the globe, our country and our communities. We responded by quickly transforming from a traditional mental health center to a digital environment, where people could continue to access and receive services, which have been especially needed during this traumatic, historic time. If those in need of care did not have a smart phone or computer to access teletherapy, we provided them with the technology they required, with ongoing service at no charge. In addition to video therapy and/or therapy-by-phone, other new services were launched, including a support/warmline and a client tracker system to outreach to new and existing clients who did not/could not/would not receive services virtually and needed to continue to be seen in-person during COVID-19.
In a world with so much change and upheaval, communication and messaging becomes a lifeline, and we quickly shifted platforms, positioning and content to reach people where they were – at home and online. A digital Mental Health Care Kit on MindSpringsHealth.org sought to be a comprehensive curation of as many important resources that we and our partners could provide. Over the course of 67 days, 52 live events were held on Facebook – offering 27 different, relevant-for-COVID-times support, like Coping Skills, Meditations, Parenting during COVID, Anger Management, Resiliency, Mindful Eating, Kid-focused Skills & Activities, Support for Essential Workers and more to our communities and those stressed during the Pandemic.
During the initial Peace in the Pandemic period from March through May,
Our digital posts reached 187,042 individuals and engaged nearly 24,000
Video views were up 1,743% from previous period to 47,400
People spent over 420 hours viewing the events, an increase of 3,087% from previous times
Thanks to a grant from the Federal Emergency Management Agency (FEMA), Mind Springs Health activated a COVID-19 recovery program to provide those impacted by the coronavirus with community-based outreach, stress reduction and resilience education and connection to mental health and other community resources.
Local outreach specialists support and educate individuals, groups and organizations impacted by the pandemic in problem solving, prioritizing needs and improving communication skills, thereby empowering self-advocacy. The program is available at no cost to all COVID-19-impacted Coloradans and all connections are done in a COVID-19 appropriate manner. Weekly virtual support groups for middle and high schoolers, caregivers, those dealing with grief and loss, and sessions held in Spanish are some of the most popular programs offered by the 12-person Colorado Spirit team directed by Amy Gallagher, PsyD, a Mind Springs Health vice president.



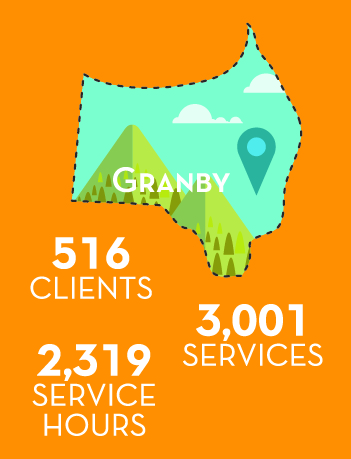
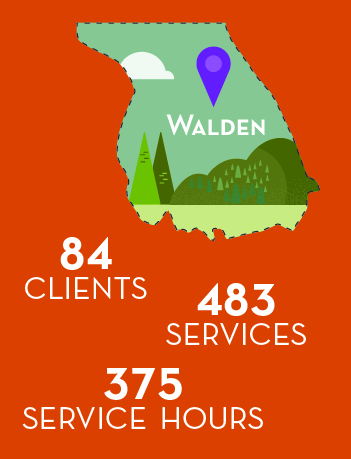
Covering over 500,000 residents across 23,000 square miles and 10 counties with a comprehensive array of services including Metricovery™, an award-winning treatment for depression and mental illness.



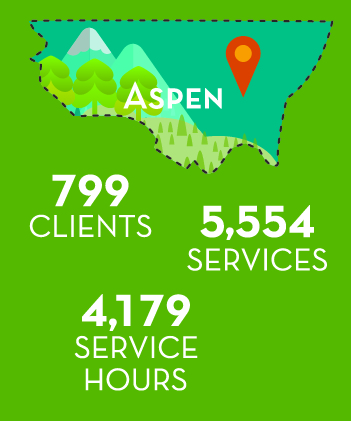
Starting in 2019, Mind Springs Health has been proud to be a part of the PACT program in Pitkin County. PACT stands for Pitkin Area Co-Responder Teams, a collaborative community program between law enforcement and mental health professionals. The co-responder team jointly responds to calls where substance abuse and/or mental health challenges may exist and consists of a licensed mental health clinician, local police officers and deputies from Aspen Police Department, Snowmass Village Police Department, and Pitkin County Sheriff’s Office, a case manager and peer specialist.
PACT’s goals are to decriminalize mental illness, reduce incarcerations of low-level offenders with mental illness, decrease emergency room visits for mental health care and reduce repeat police calls for individuals in need of community-based services and mental health support.
 On scene, the mental health co-responder works with officers and deputies to help stabilize the situation and to develop a plan to help. A full-time case manager follows up after the co-response and manages the plan. This may involve helping with transportation to doctor appointments, making sure they get their medications, helping navigate legal issues, assisting with access to economic assistance or other community services, coordinating access to counseling, group support, and/or treatment, and providing resources to loved ones for another layer of support.
On scene, the mental health co-responder works with officers and deputies to help stabilize the situation and to develop a plan to help. A full-time case manager follows up after the co-response and manages the plan. This may involve helping with transportation to doctor appointments, making sure they get their medications, helping navigate legal issues, assisting with access to economic assistance or other community services, coordinating access to counseling, group support, and/or treatment, and providing resources to loved ones for another layer of support.
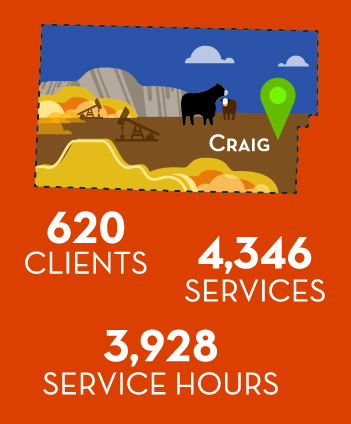
 A longtime therapist in the office and frequent ‘Customer Service Superstar’ nominee, Peggy Sammons LPC was named Moffat County Program Director. Together with Peer Specialist Sheryl Zulian, Peggy is helping further integrate our services into the community. This fiscal year, the award-winning measurement & phase-based care program MetricoveryTM became available in the Craig office and the successful Peer Support Special program assisted local residents through shared experiences.
A longtime therapist in the office and frequent ‘Customer Service Superstar’ nominee, Peggy Sammons LPC was named Moffat County Program Director. Together with Peer Specialist Sheryl Zulian, Peggy is helping further integrate our services into the community. This fiscal year, the award-winning measurement & phase-based care program MetricoveryTM became available in the Craig office and the successful Peer Support Special program assisted local residents through shared experiences.

Eagle County Program Director Chris Rieder LPC, Program Coordinator Melissa Riggins and the entire 30-person Eagle County Mind Springs team work closely with Eagle Valley Behavioral Health to transform mental health in the valley. From Business Services Associate Eric Sunblad to Community-based Intensive Treatment Team (CBITT) member Dawn Nichols, the team continuously adapts to the changing landscape of local community need.
 With the addition of Dr. Patrick Sassoon, a trilingual psychiatrist, to the team, Spanish-speaking clients can now receive psychiatric services in their native language.
With the addition of Dr. Patrick Sassoon, a trilingual psychiatrist, to the team, Spanish-speaking clients can now receive psychiatric services in their native language.

This year, Mind Springs Health in Summit County moved to a spacious new office in the Summit Daily building at 301 West Main Street and welcomed a new Chief Medical Officer based out of the Frisco office. Dr. Will Elsass specializes in child and adolescent psychiatry and has brought a broad range of experience to Mind Springs Health, having worked in medical administration and as a psychiatrist in both private practice and in the United States Air Force. Joining us in March just before the pandemic took off, Dr. Elsass was the chief architect of our infection control program in our effective pandemic response plan and a main provider for our urgent psychiatric care clinic.

Self Care is Important to Relieving Stress and Anxiety
By William Elsass, MD

Program Director Hans Lutgring, Program Coordinators Tammy Perry & Annie Edgecombe and Psychiatrist David Conklin MD head up Mind Springs Health’s Garfield County office and partnerships. After nearly 25 years on the outskirts of town, Mind Springs Health is making plans to relocate to a more central Glenwood Springs location at 2802 Grand Avenue, and participating in talks regarding restoring a social detox to the community.
 Mind Springs Health is very appreciative of the Grand County community and their leadership in supporting our team as the County’s crisis services responder. Program Director Makena Line, along with clinicians Cynthia James MSW and Lance Howe MSW CAC III, also seamlessly provide comprehensive mental health services to the community both pre- and now during the pandemic.
Mind Springs Health is very appreciative of the Grand County community and their leadership in supporting our team as the County’s crisis services responder. Program Director Makena Line, along with clinicians Cynthia James MSW and Lance Howe MSW CAC III, also seamlessly provide comprehensive mental health services to the community both pre- and now during the pandemic.
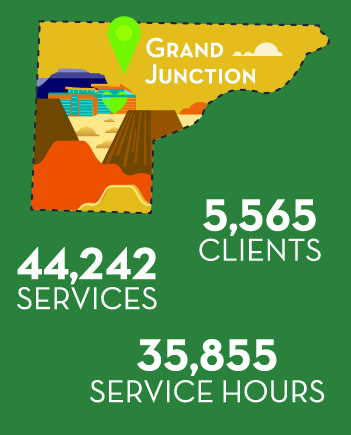
The pandemic has been taking an increased toll on our individual and collective mental health and is responding both in traditional and new ways. Our Mesa County-based clinicians hold two ‘Pop-Up’ clinics weekly in the community and now offer a hybrid of access to services to help ensure clients receive services in the format they feel most comfortable.
Suicide remains a serious challenge to the community, and a recent study from the Educational Fund to Stop Gun Violence found that in 2018, 77% of all firearm deaths in Colorado were suicides. In addition to our participation in the nationwide Zero Suicide initiative, we actively work on reducing access to lethal means in the community.

 For most of the year Mind Springs Health in Rio Blanco county continued to provide crisis response services 24/7 and was fully staffed with 3 clinicians including Program Director Michelle Huber CAC III. In addition to evidence-based therapies and services, Rio Blanco residents benefited from a number of Mind Springs Health’s complimentary resiliency and mental health first aid trainings prior to the pandemic. During the coronavirus, all services are available virtually
For most of the year Mind Springs Health in Rio Blanco county continued to provide crisis response services 24/7 and was fully staffed with 3 clinicians including Program Director Michelle Huber CAC III. In addition to evidence-based therapies and services, Rio Blanco residents benefited from a number of Mind Springs Health’s complimentary resiliency and mental health first aid trainings prior to the pandemic. During the coronavirus, all services are available virtually


The Mind Springs Health’s Routt County team expanded their services amid the pandemic. Special recognition is extended to bilingual Business Services Associate Grasiela Michaels, who does a superlative job participating in daily clinical meetings, supporting our other offices, outreaching clients and developing and nurturing strong connections with our partner agencies and referrers.

Still mourning our beloved Jane Bingham, Mind Springs Health in Jackson County has persevered in supporting the community’s mental health and substance use challenges and recent accomplishments placed mental health support in both the school and the jail. Program Coordinator Tammy Gildenzoph is in the office every Tuesday through Thursday, and Business Services Associate Sheri Geer won a “Going Above and Beyond” award this year in recognition of her client care.
Substance use disorders and mental health conditions often go hand-in-hand, and addressing both addiction and the underlying causes for addiction are key to successful recovery.
The Women’s Recovery Center is a healing, women-only intensive drug and alcohol treatment and transitional living program, specializing in holistic recovery. One of the most unique aspects of the Women’s Recovery Center is that the residents are able to have their children (under the age of 10) stay with them during their time at the Center. Often times, this means children are kept out of the foster care system, while also providing their mothers with the comfort of knowing their children are safe so they can better focus on the healing process.


Each resident has a personal addiction counselor for one-on-one therapy and guidance. Daily schedules are highly-structured and focus upon personal responsibility and empowerment as well as the dynamics of addiction, relapse and recovery.
After many years on the Grand Junction Regional Center Riverside Parkway campus, The Women’s Recovery Center spent this past year planning, designing and constructing a new facility on 7 acres in Clifton, CO. The Center moved into the new building just after the end of the fiscal year and Jordan and Marley were special guests and featured speakers at the Grand Opening celebration. In addition to spacious grounds for outdoor activities like walking the meditation path, the new campus supports new therapy programs like light, horticultural, and 3-D virtual therapies, and exercise therapies like yoga and weight training.
Meet Jordan Shaw, a proud graduate, and her daughter Marley.
3,440 Total Crisis-related Contacts

As of September 2019, Mind Springs Health has been contracted by Rocky Mountain Health Plans as the Colorado Crisis Services mobile responder for Grand, Jackson, Mesa, Moffat, Pitkin, Rio Blanco and Routt counties, along with parts of Garfield County. Crisis services throughout the State are accessed by calling the Colorado Crisis Services hotline at 1. 844.493. TALK or texting TALK to 38255. Hotline clinicians then alert our teams to respond if/when further contact is warranted.



The new West Springs Hospital opened 2018 with 48 new beds and a special children and adolescents unit to accompany 16 remaining beds in an older building. This older unit, detached from the new Hospital, has extended its life as a self-contained COVID-19 unit, ensuring everyone gets the psychiatric help they need, while keeping ALL patients and staff healthy and safe during the pandemic.
Admissions are accepted 24/7/365 and a center for walk-in assessments is available 23/7 (all day/night except between 4-5a).
As many know, we are the only psychiatric hospital in Western Colorado. But few know what defines an excellent psychiatric hospital and what makes West Springs excellent. We are not just any typical rural mental health facility. For starters, people need to feel safe. Our 21st century hospital has the most modern and latest safety features available in the world – ranging from the choice of door hinges and handles to the geographic layout of the nursing stations. Many people with psychiatric disorders have experienced a range of traumas and stresses in their lives and feeling safe additionally means that staff are trained in this fact. Our work culture inculcates ‘trauma-informed treatment’ into everything that we do.
People shouldn’t feel trapped in hospitals. Our hospital is blessed to have a wide range of windows and access to natural light. There are also outdoor spaces that are enclosed within the hospital campus that allow people access to fresh air and sunshine. There is room to stroll. Having a gym is obviously helpful for exercise, but is also an alternative place to go for patients who are feeling confined. People need to feel hope and to grow and the hospital is designed and the employees are trained to let that happen.
People need to feel that their illness is well-treated. Admission to a hospital means that there is an illness, and that it requires treatment. Diagnosis and treatment of psychiatric illness is a rapidly progressing field, with daily advances in neuroscience and our understanding of mental disease. We have recruited staff from across the country providing a broad range of proficiency, skills and knowledge and allowing us to be a source of expertise in psychiatry.
Relatedly, we are a training ground for many of the psychiatric providers on the Western Slope.
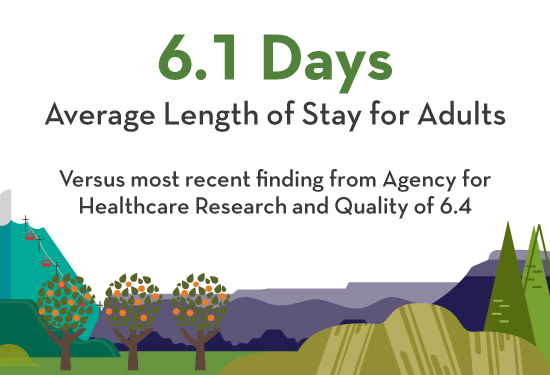
But recovery is not just lying in bed and waiting for the medications to work. We are also notable for the depth of therapeutic activities in which patients can be involved on a daily basis. Tailored therapies may range from one-on-one to group, exercise, yoga, music and/or play etc., and we are staffed to provide this individualized attention to recovery. Nonetheless, we know that hospitalization is just one step in the road to recovery. Many are surprised to find that the average length of hospitalization is six days – with most recovery occurring outside the hospital.
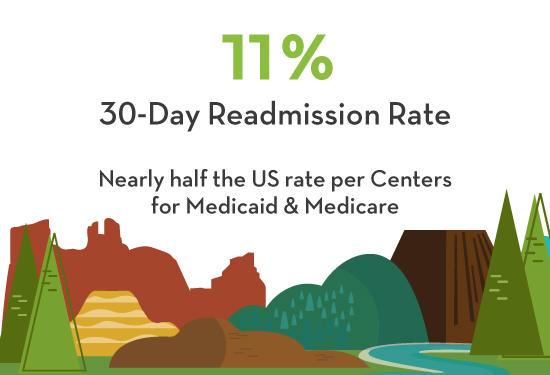
Integrating hospitalization with ongoing outpatient care, furthering collaborative activities amongst a variety of stakeholders and coordinating that care can be challenging . We are meeting that challenge, pioneering providing clinical information access to other physicians, and breaking down the barriers between psychiatric care and medical care. Proof of our success in integrating collaborative care is our low readmission rates; we are easily in the top 1% in the United States. This numerical success comes about because of our abilities in integrating our care with the many other levels of care outside of the hospital.
We care for our patients with the utmost respect, and are appreciative of trust placed in us every day.




The need for the newly created Mind Springs Foundation arose long before COVID-19 made its way into our communities and lives; however, the arrival of the new entity was timely as the need for behavioral healthcare continues to increase throughout Western Colorado.
In 2019, the decision was made to create a new 501(c)(3) to serve as the philanthropic arm of Mind Springs Health and West Springs Hospital, and the entity became a reality in 2020. All financial gifts to Mind Springs Health and/or West Springs Hospital are now directed and received through the Foundation. Donors can still designate where their investments are directed, whether they choose to support West Springs Hospital, Women’s Recovery Center, a local Mind Springs Health office or other vital behavioral health program.
Led by Mind Springs Foundation President Roger Sheffield, the Foundation team is focusing fundraising efforts on:
The Mind Springs Health Board of Directors and the West Springs Hospital Board of Directors are comprised of a core group of seven directors who serve on both Boards, with four additional directors per board. This past fiscal we welcomed Karin Van Meter to the Mind Springs Health Board of Directors and Jim Cleaver to the West Springs Hospital Board.
AL SALIMAN, MD, Chair
Health Care
Garfield County

PAT TUCKER, Chair-elect
Real Estate Development
Mesa County

CAROL SKUBIC, Secretary/Treasurer
Finance
Mesa County
BILL ANUSZEWSKI, MBA
Finance
Pitkin & Garfield Counties
BILL NOEL
Health Care
Garfield County
ANGELA STRODE
Legal
Garfield County
SHARON RAGGIO, LPC LMFT MBA
President & CEO
Mind Springs Health
& West Springs Hospital
STEFAN BATE, LAC CCTP
Health Care
Roaring Fork Valley
MARK SCHEEL
Technology
Vail Valley
KARIN VAN METER
Health Care
Mesa County
Reverend CARL WALKER
Retired
Vail Valley
JIM CLEAVER
Education
Garfield County
LARRY DUPPER
Health Care
Garfield County
STACEY GAVRELL
Health Care
Garfield County
JOAN NAPOLILLI, RN MSN
Health Care
Montrose County

SHARON RAGGIO, LPC LMFT MBA
President & CEO
SRaggio@MindSpringsHealth.org

DOUG PATTISON, CPA
Chief Financial Officer
DPattison@MindSpringsHealth.org

WILLIAM ELSASS, MD
Chief Medical Officer
WElsass@MindSpringsHealth.org

ROGER SHEFFIELD
President, Mind Springs Foundation
RSheffield@MindSpringsFoundation.org

KIM BOE, ACHE HRM
Executive VP, West Springs Hospital
KBoe@WestSpringsHospital.org

MICHELLE HOY, LPC CAC III
Executive VP, Mind Springs Health
MHoy@MindSpringsHealth.org
AMY GALLAGHER, PsyD
VP
CHRISS P. FLYNN
VP, Marketing
DAWNELLE SAWYER, MSN RN CMHP
Director of Nursing, West Springs Hospital
FRANCIS LOTRICH, MD PhD
Medical Director, West Springs Hospital
KRISTA McCLINTON
VP, Informatics
STEPHANIE KEISTER
Manager, Public Relations
AUDREY KISER
Director, Data Analytics
COLETTE ROSQUIST, LCSW
Director, Social Services, West Springs Hospital
ELIZABETH TICE
Managing Director, Budgeting & Finance
JACKIE SKRAMSTAD, LCSW
Manager, Mind Springs Health Clinical Operations
LYNN MANAHAN
Managing Director, Enterprise Revenue
TOM GANGEL
Manager, Training & Community Outreach
BRANDI KROESE, CAC III
Director, West Springs Hospital Operations
DAVID HAYDEN, LPC CAC III
VP, Quality & Compliance
FELICIA ROMERO, LPC CAC III
Manager, Crisis Programs Operations
KATHY CAPPS, LPC LAC
Director, Mind Springs Health Operations
NORMA ROBERTS
VP, Human Resources
We rebuild lives and inspire hope by providing exceptional mental health
and addiction recovery care, strengthening the health and vitality of our communities.
We envision health and wellness in our communities.
Strength Created through Local Partnerships, with Collaboration and Education
Integrity and Accountability in all we do
Outcomes-Driven
Responsible Financial Stewardship
Leadership in Physical and Behavioral Health Care
A Culture of Trauma-Informed Care
A Focus on Exceptional Customer Service
Our Workforce, for its Compassion and Dedication to the Fulfillment of our Mission
The Delivery of Services and Operations that Promote Social Equity across all Stakeholders
